Kidney Stones
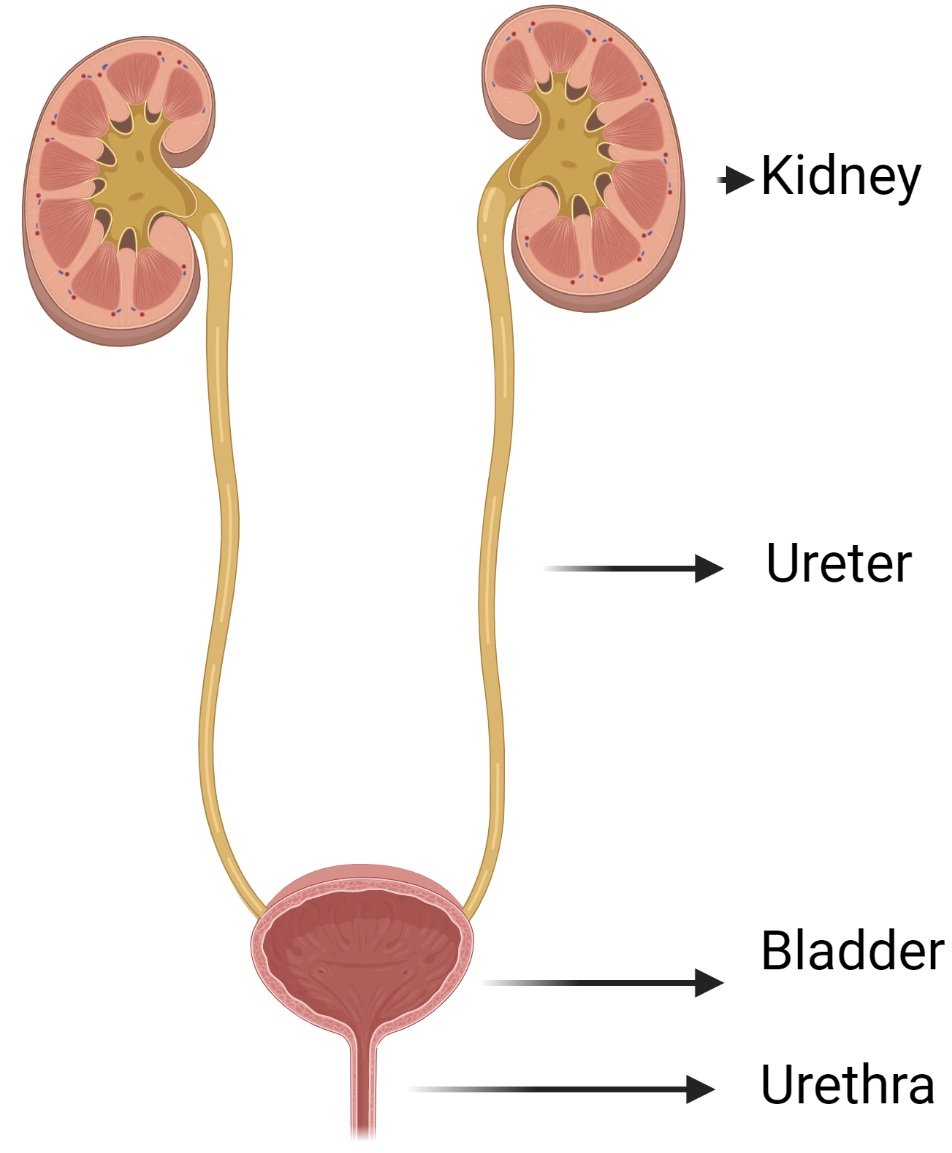
Diagram of the urinary tract
What causes kidney stones?
Kidney stones are a common medical condition. 5% of women and 13% of men will have kidney stone at some point in their life. It is associated with the rise in obesity and type 2 diabetes. The type of kidney stones varies by geography and genetics. In Australia, the most common type is calcium oxalate (with or without phosphate), followed by uric acid stones, then infection related stones.
Stones form when the urine becomes oversaturated with stone components. The components stick together, forming a complex. These complexes then become anchor points to grow, much like a snowball rolling downhill as the stone gets larger and larger.
There are other factors which affect kidney stone formation. This includes urine pH and genetic predispositions which code for instance calcium and phosphate reabsorption from the urine. A higher amount of calcium and phosphate in the urine leads to stone growth.
How can I prevent kidney stones?
As general guidelines, people with kidney stones should:
1. Increase fluid intake to at least 2-2.5 litres each day – And of course more in summer. Fluid dilutes out the stone constituents. People with cystine stones sometimes require a urine output of 4 litres per day to prevent stone formation! It makes sense that the maximum risk for stone formation is at night when urine concentration is at its highest. Nearly any fluid will do, including water, coffee, tea, and alcohol (in moderation of course).
2. Consuming citrus juices may help by alkalinising urine and increasing citrate in the urine. The evidence for this is mixed. The studied doses of citrate are the equivalent of around 1.2L of orange juice, or 120mL concentrated lemon juice (which can be found in supermarkets and mixed with 1-2 litres of water) each day
3. Limit daily sodium intake to 2g per day – This is around a teaspoon of table salt per day - Much of the salt intake in our diet is hidden so I encourage my patients to look at the labels of foods they buy. This is especially important in processed foods. High intake of sodium increases urine sodium which also increases urine calcium. High urine calcium predisposes to calcium stones.
4. Have high calcium foods – Intuitively a decreased calcium intake should decrease urine calcium and therefore lower chances of stones. However calcium binds to oxalate in the gut where is passes through our bowel motions. This therefore decreases urine calcium and stone production. I would suggest calcium from dietary sources rather than supplements. This is because supplements introduce a large instant amount of calcium which may be rapidly absorbed and passed into the urine.
5. Avoid animal protein – These proteins tend to make the urine more acidic, increases urine uric acid and urine calcium. This favours calcium and uric acid kidney stone formation. Be aware that meat substitutes such as Quorn still have a significant amount of protein that can cause kidney stones. Therefore avoid this in those with oxalate and uric acid stones
Further diet detail can be given by your kidney specialist and dietician depending on your stone type.
Preventative medications your doctor prescribes depend on further tests. For example:
· For high calcium in the urine, a thiazide may be given to increase reabsorption back into the bloodstream
· For high oxalate in the urine, vitamin B6
· For those with acidic urine, potassium citrate to help alkalinise the urine. This can be important in calcium oxalate and uric acid stones
· For those with uric acid stones, allopurinol (you may be on this already for gout)
What are the symptoms of kidney stones?
Patients with kidney stones often experience “renal colic”. This is sudden and intense pain in the sides that radiate down into the pelvis, so called “loin to groin” pain.
Other symptoms may include blood in the urine, increased urge or frequency of urination, nausea and vomiting. On passing a stone, my patients often describe a feeling of passing sand.
Some people do not have symptoms. Stones may be found incidentally, for example imaging the abdomen for other reasons.
How is a kidney stone diagnosed?
Usually a stone can be suspected on the basis of symptoms.
After this, we usually confirm the presence of stones through imaging. This can be done either through pairing a kidney ultrasound and xray of the abdomen; or through CT scanning.
While waiting for stones to pass, you may be encouraged to urinate through a strainer. This is to catch the stone, which is then sent for analysis. Knowing your stone type is useful in knowing how to prevent future stones.
What are the treatment options for kidney stones?
Many people with kidney stones can be managed at home with pain medications and hydration.
A medication called tamsulosin may be prescribed to speed the passage of the stone. This may be useful in those who look like they are able to pass the stone. An example is a 5-10mm stone that has been able to make it all the way down the ureter and close to the bladder.
There are a few people who need hospitalisation and/or surgery however, including:
· Those unable to keep food or fluid down, for example because of nausea
· Uncontrollable pain
· Fever – This may be a sign of an infected stone
· Those who stop passing urine. For example stones may block both kidneys simultaneously causing kidney failure
· Stones that do not pass after a few weeks – Usually these stones are quite large (>1cm diameter)
Surgical options to remove stones may include:
· Shock wave lithotripsy – An ultrasonic energy beam is shot through the skin to break up the stone.
· Ureteroscopy – A camera is passed up through the urethra, bladder, then up into the ureter. The stone can be retrieved or a laser can be fired at the stone to break it up
· Percutaneous nephrolithotomy – This is where the kidney is cut open to retrieve the stone. This is useful for large stones over 2cm
How can I manage the pain of kidney stones?
For pain control during an episode of renal colic, paracetamol and anti-inflammatories have proven to be effective within an hour of taking them. In addition to an anti-inflammatory effect, these medications help relax the ureter, in turn decreasing spasm. Anti-inflammatories also have less side effects compared with opioids such as oxycodone and morphine. This includes nausea, vomiting, confusion and constipation.
Examples of anti-inflammatories include ibuprofen (also called Brufen, Nurofen, Advil) and diclofenac (also called Voltaren). If a person is too nauseous to take tablets, an injection form can be used instead.
Can drinking water help pass a kidney stone?
Increased fluid intake is well studied to prevent kidney stones. However the effectiveness of high fluid intake in those having an active episode of kidney stones is unclear. While drinking more may help “flush” the stone out, there have been some studies done showing that there is no change in ureter pressure to try and expel the stone.
On balance of the evidence, there is little downside drinking more fluid as long as it does not build up on you!
How long does it take to pass a kidney stone?
The likelihood of ureteral stones passing without intervention depends on their size and location. Smaller stones are more likely to pass, especially those less than 0.5cm diameter. Depending on the study, stones ≤0.2cm in diameter take an average of around a week to pass. Between 0.2 and 0.4cm, around 2 weeks, between 0.4 and 0.6cm, around 3 weeks. Those greater than 1cm are unlikely to pass by themselves.
Another sign that the stone is likely to pass is how far they pass through the kidney system. Progress of stone passage can be done through serial imaging. If progress imaging demonstrates that the stone has made it down the ureter and into the bladder over time, then these stones are more likely to pass than imaging which demonstrates a stone that is still stuck quite high up near the kidney.
Can kidney stones cause permanent damage?
Passing kidney stones can be quite painful. However usually no permanent damage is caused if recognised on time.
In the long term, a stone left obstructing a kidney will cause that kidney can fail. These kidneys shrivel up as they fail. I have occasionally scans with one healthy kidney, and a shrunken kidney with a stone in it!
Sources:
Johnson Richard J John Feehally and Floege Jürgen. 2019. Comprehensive Clinical Nephrology (version Sixth edition) Sixth ed. Edinburgh: Elsevier. http://www.engineeringvillage.com/controller/servlet/OpenURL?genre=book&isbn=9780323479097>
Lee, MC., Bariol, S.V. (2012). Epidemiology of Stone Disease in Australia. In: Talati, J., Tiselius, HG., Albala, D., YE, Z. (eds) Urolithiasis. Springer, London.
Stoller, Marshall L. and Maxwell V. Meng. “Urinary stone disease : the practical guide to medical and surgical management.” (2007).
UptoDate